
Medicare has finalized its second round of drug price negotiations, covering 15 widely used medicines and delivering cuts as deep as 71% for some medications. This marks a historic moment in American healthcare, for the first time in decades, the government is using its purchasing power to bring down prescription drug costs for seniors.
While these lower prices won’t arrive until 2027, the implications are enormous for millions of Americans struggling to afford their medications.
Here’s What Just Happened

Medicare just negotiated prices for 15 expensive medications, including the blockbuster weight-loss drug Ozempic. The government secured price cuts ranging from 38% to a stunning 85%, with some drugs dropping by more than two-thirds. This is the second round of negotiations under the Inflation Reduction Act, and it’s a game-changer for seniors struggling with high medication costs.
According to the Centers for Medicare and Medicaid Services, “By making drugs more affordable, the program can improve health outcomes. When patients are better able to afford their medications, they’re more likely to take them consistently.” The price cuts won’t take effect until 2027, but when they do, millions of Americans could see major savings on some of the most popular drugs in America.
The 71% Drop
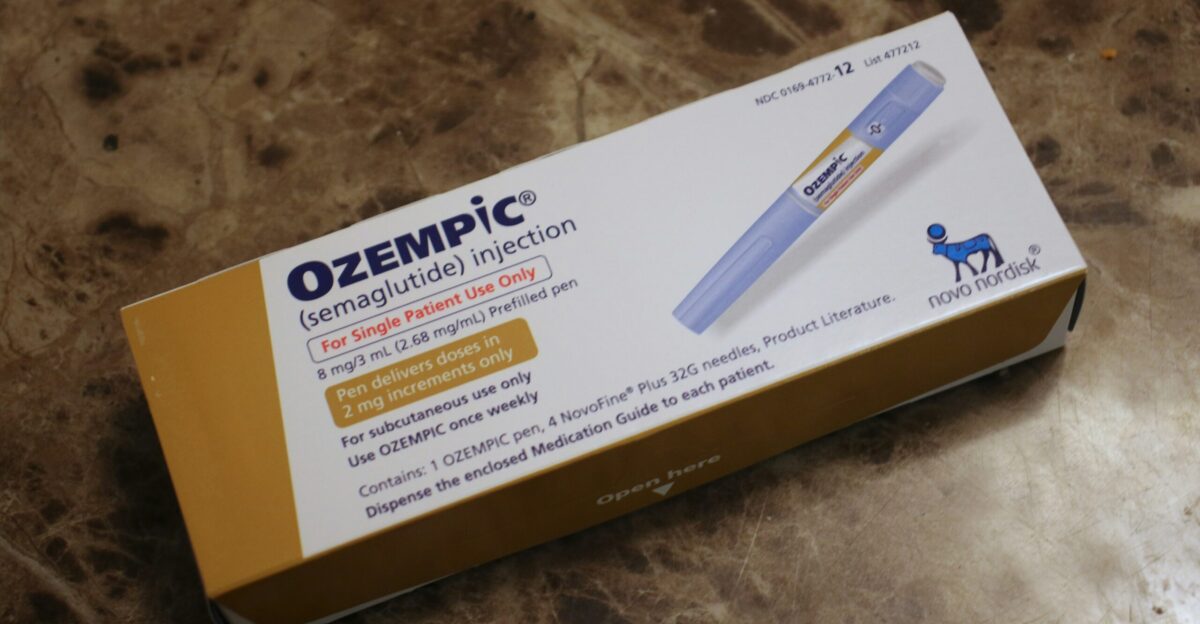
Two of America’s most talked-about drugs, Ozempic for diabetes and Wegovy for weight loss, are getting a massive price reduction. Right now, these medications cost nearly $1,000 per month. Under the new Medicare deal, they’ll drop to about $274 per month. That’s a yearly savings of roughly $8,700 for each patient.
Even if insurance plan details mean you don’t save the full amount, Medicare expects seniors to collectively save hundreds of millions of dollars. Patients on fixed incomes will finally be able to afford to take their medications consistently without rationing doses.
Which 15 Medications Are Getting Price Cuts?

The negotiated drugs treat serious conditions including diabetes, cancer, asthma, leukemia, and Huntington’s disease. They were chosen because they have no generic competitors and cost Medicare enormous sums. The deepest cut of 85% goes to Janumet, a diabetes medication.
Other big discounts include Ozempic and Wegovy at 71%, while Austedo for Huntington’s disease gets a 38% reduction. These drugs were picked specifically because they’re expensive, widely used by seniors, and have limited cheaper alternatives.
A $12 Billion Save

If these negotiated prices had been in place during 2024, Medicare would have spent $12 billion less on these 15 drugs alone, far more than the first round of negotiations saved. About 5.3 million Medicare patients currently use at least one of these drugs, meaning the average savings will reach around $2,000 to $2,400 per person per year.
Seniors themselves will save approximately $685 million annually in direct out-of-pocket costs. For the government and taxpayers, that’s a massive reduction in spending. For families already stretching budgets thin, these savings could mean the difference between buying food and buying medicine.
Good News Has a 16-Month Delay

Here’s the frustrating part: the new lower prices don’t start until January 1, 2027. That means more than 50 million Medicare beneficiaries must wait roughly 16 more months and continue paying high prices. For people on fixed incomes, this wait can be crushing.
The choice between paying close to $1,000 monthly for medication or skipping doses becomes real and dangerous. Some patients will abandon treatment altogether, risking disease progression and more expensive hospital visits.
Breaking a 20-Year Prohibition

For two decades, Medicare was legally banned from negotiating drug prices with pharmaceutical companies. That changed with the Inflation Reduction Act in 2022, which finally gave Medicare the power to bargain for better deals. The law created a rolling schedule: ten drugs got negotiated prices starting in 2026, and now this second batch of 15 drugs kicks in for 2027.
More drugs will be added to the program each year. This was a historic shift in how America buys medicines. Drug companies fought the law hard, but supporters argued that if other wealthy countries can negotiate prices, so can America’s government.
Medicare’s Price vs. Trump’s Deal

Here’s where things get complicated. In November 2025, the Trump administration announced a separate agreement with Novo Nordisk and Eli Lilly for their GLP-1 obesity drugs. Under this deal, Ozempic and Wegovy would cost just $245 per month, $29 cheaper than Medicare’s negotiated $274.
This side deal applies to Medicare and Medicaid beneficiaries starting in 2026, a full year earlier than the Medicare negotiation prices. Health policy experts are confused about which price will actually apply when both agreements are in effect. Companies say they need clarity from federal regulators, and nobody’s sure how this patchwork of overlapping deals will work in practice.
What This Means for Your Wallet

For a Medicare patient taking Ozempic continuously, moving from $1,000 monthly to $245 or $274 means saving between $8,700 and $9,000 per year. For seniors living on Social Security checks, that’s a life-changing difference. But the benefits go deeper. When medications cost less, people actually take them as prescribed instead of rationing doses.
That consistency prevents serious complications like heart disease, kidney failure, and vision loss. Fewer complications mean fewer expensive hospital visits, emergency room trips, and surgeries. Lower medication costs today can mean better long-term health and fewer costly medical emergencies down the road for both patients and the healthcare system.
Cancer and Other Serious Diseases

While Ozempic gets all the headlines, the negotiation includes vital cancer treatments, leukemia medications, and asthma drugs. These therapies previously consumed huge portions of Medicare’s budget because they had little competition and historically avoided big discounts.
Cancer patients, in particular, depend on these life-saving drugs and often face crushing costs. The negotiated price cuts for oncology and blood cancer treatments are especially significant because these drugs are often the difference between life and death.
Who’s Backing This Deal?

Major organizations supporting these price cuts include AARP, which represents about 125 million Americans over 50. Both Democratic and Republican administrations have backed the negotiation program, though for different reasons.
CMS officials emphasize that after decades under a system that prevented Medicare from negotiating, this second round marks a major victory in curbing prescription drug prices.
The Selection Process Explained

The process to pick these 15 drugs was rigorous and data-driven. CMS started by identifying medications that have been on the market for years, have no generic or cheaper biosimilar alternatives, and eat up huge chunks of Medicare spending. Officials then worked through structured negotiations with manufacturers, requesting pricing data and studying effectiveness.
The second round achieved larger total savings than the first because it targeted several high-cost cancer medications and GLP-1 drugs, and CMS used lessons learned from the initial negotiations to improve their strategy. The selection method ensures that the negotiation program focuses on drugs where it can deliver the most benefit to patients and save the most money for the system.
What Drug Companies Are Saying

Pharmaceutical companies have vigorously opposed the negotiation program and filed multiple lawsuits, claiming it amounts to unconstitutional price controls. They argue that forced discounts will reduce profits available for research into new drugs, potentially slowing medical innovation.
However, health economists counter that negotiated prices still remain well above production costs and leave room for substantial profits. They point out that the 71% Medicare discount for Ozempic doesn’t apply to commercial insurance or uninsured patients, so companies still earn huge revenues from other markets.
Lawsuits and Uncertainty

Drug manufacturers have already filed multiple lawsuits challenging the negotiation program’s constitutionality, and more litigation is expected as additional high-revenue drugs enter future rounds. Federal courts will eventually decide whether Congress had the power to let Medicare negotiate drug prices.
Meanwhile, analysts warn that overlapping Trump-era arrangements, future regulatory guidance, and potential court rulings could reshape how these negotiated prices actually work in practice. Some policies could be overturned, while others might be strengthened depending on court decisions and political changes.
Who Gets Help?

Roughly 5.3 million Medicare beneficiaries currently use at least one of these 15 negotiated drugs, so roughly 10% of America’s 50-plus million seniors will be directly affected by these price changes. If even a fraction sees the full benefit of lower prices, millions of people will experience genuine relief from medication costs.
The average savings per affected patient could reach $2,000 to $2,400 annually, translating to thousands of dollars per household per year. For seniors already struggling with rent, food, and utilities, this relief means they can prioritize health without sacrificing basic living expenses.
A New Era in American Healthcare

For decades, seniors had no choice but to accept whatever prices pharmaceutical companies demanded. The 2022 Inflation Reduction Act finally gave Medicare permission to negotiate, breaking a 20-year legal ban. This second round of negotiations signals that Washington is genuinely willing to challenge Big Pharma’s pricing power.
Future rounds will bring even more drugs into the negotiation process, eventually covering a substantial portion of Medicare’s drug spending. While legal challenges continue and political winds may shift, the fundamental change, that government can and should bargain for better drug prices, appears here to stay.
Sources
- Centers for Medicare & Medicaid Services. (2025, November 24). CMS delivers savings for seniors on 15 major drugs. U.S. Department of Health and Human Services. Retrieved from
- CMS Deputy Administrator and Medicare Director Chris Klomp. Statement on Medicare Drug Price Negotiations Program. (2025, November 24). Retrieved from CMS official communications.
- Robert F. Kennedy Jr., Health and Human Services Secretary. (2025, October 29). Remarks on FDA drug approval changes and drug pricing reforms. Retrieved from HHS press room communications.
- Centers for Medicare & Medicaid Services. (2025, November 26). Clarification on most-favored-nation pricing vs. IRA-negotiated prices. CMS Statement on GLP-1 drug pricing. Retrieved from CMS newsroom.


